MISSION AND VISION
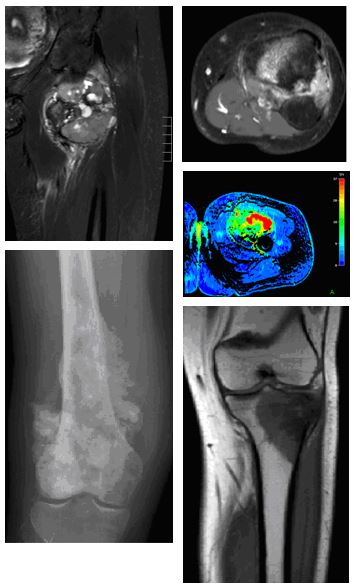
Musculoskeletal (MSK) tumours are rare and comprise a multitude of diverse entities. Recognition and early, accurate diagnosis of bone and soft tissue sarcomas are crucial for satisfactory patient outcomes. Bone and soft tissue tumour imaging is a mainstay of the diagnostic MSK tumour work-up. Standardized algorithms should be followed for local staging, and, if needed, for whole-body assessment, as well as for therapy control and follow-up.
The ESSR subcommittee Tumours consists of a group of colleagues who have a particular interest and expertise in imaging of musculoskeletal tumours, of both bone and soft tissues.The group was founded in 2005, with Suzanne Anderson as the subcommittee chair (three-year term), and “Pater” Mark Davies, Hans Bloem, and Daniel Vanel, and a great group of enthusiastic colleagues with representatives from many European countries.
The intention of the group is to promote both educational and research issues in bone and soft tissue tumours. This includes the standardization of imaging algorithms, and better understanding of imaging findings, as well as multicentre studies.
The subcommittee organizes the refresher session “Tumour Imaging” at the ESSR annual meeting.
CHAIRPERSON
Chairperson
Violeta Vasilevska Nikodinovska, Skopje/MK
Vice-Chairperson
Slavco Ivanoski, Ohrid/MK
CHAIRPERSON
Past Chairpersons
Radhesh Lalam, Oswestry/UK
Marc-André Weber, Heidelberg/DE
Iris-M.Noebauer-Huhmann, Vienna/AT
Carla S.P. van Rijswijk, Leiden/NL
Joan C. Vilanova, Girona/ES
Suzanne E. Anderson, Sydney/AU
Members
For a list of subcommittee members, please VISIT HERE
PUBLICATIONS
Selected Recent Publications (in alphabetical order):
Publications
> Anderson SE, Johnston JO, Steinbach LS. Pseudotumors of the shoulder. Eur J Radiol. 2008; 68:147-58.
> Anderson SE, Steinbach LS, Schlicht S, Powell G, Davies M, Choong P. Magnetic resonance imaging of bone tumors and joints. Top MagnReson Imaging. 2007; 18:457-65.
> Azura M, Vanel D, Alberghini M, Picci P, Staals E, Mercuri M. Parosteal osteosarcoma dedifferentiating into telangiectatic osteosarcoma: importance of lytic changes and fluid cavities at imaging. Skeletal Radiol. 2009; 38:685-90.
> Bloem JL, Reidsma II. Bone and soft tissue tumors of hip and pelvis. Eur J Radiol. 2012; 81:3793-801.
> Datir A, James SL, Ali K, Lee J, Ahmad M, Saifuddin A. MRI of soft-tissue masses: the relationship between lesion size, depth, and diagnosis. ClinRadiol. 2008; 63:373-8; Discussion 379-80.
> Davies CE, Davies AM, Kindblom LG, James SL. Soft tissue tumors with muscle differentiation. SeminMusculoskeletRadiol. 2010; 14:245-56.
> De Schepper AM, Bloem JL. Soft tissue tumors: grading, staging, and tissue-specific diagnosis. Top MagnReson Imaging. 2007; 18:431-44.
> Freyschmidt J. Tumor-like diseases of the knee joint. Radiologe. 2012; 52:1030, 1032-41.
> Kloth JK, Hillengass J, Listl K, Kilk K, Hielscher T, Landgren O, Delorme S, Goldschmidt H, Kauczor HU, Weber MA. Appearance of monoclonal plasma cell diseases in whole-body magnetic resonance imaging and correlation with parameters of disease activity. Int J Cancer 2014; 135: 2380-2386.
> Kotnis NA, Grimer RJ, Davies AM, James SL. Magnetic resonance imaging appearances following hindquarter amputation for pelvic musculoskeletal malignancy. Skeletal Radiol. 2009; 38:1137-46. Epub 2009 Aug 21.
> Laffan EE, Ngan BY, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: part 2. Tumors of fibroblastic/ myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin.Radiographics. 2009; 29:e36.
> Lakkaraju A, Sinha R, Garikipati R, Edward S, Robinson P. Ultrasound for initial evaluation and triage of clinically suspicious soft-tissue masses. ClinRadiol. 2009; 64:615-21.
> Li PK, James SL, Davies AM. Tumour and tumour-like lesions of the intercondylar notch of the knee: a pictorial review. J Med Imaging RadiatOncol. 2008; 52:434-46. Review. PubMed PMID: 19032388.
> Neubauer H, Evangelista L, Hassold N, Winkler B, Schlegel PG, Köstler H, Hahn D, Beer M.Diffusion-weighted MRI for detection and differentiation of musculoskeletal tumorous and tumor-like lesions in pediatric patients.World J Pediatr. 2012; 8:342-9.
> Noebauer-Huhmann IM. [SOFT TISSUE TUMORS: IMAGING STRATEGY FOR LOCAL PRIMARY DIAGNOSTICS – MANIFESTATION, PEARLS AND PITFALLS IN MRI]. Radiologe. 2014 Aug; 54(8):803-18.
> Noebauer-Huhmann IM, Amann G, Krssak M, Panotopoulos J, Szomolanyi P, Weber M, Czerny C, Breitenseher M, Grabner G, Bogner W, Nemec S, Dominkus M, Funovics P, Windhager R, Trattnig S.
USE OF DIAGNOSTIC DYNAMIC CONTRAST-ENHANCED (DCE)-MRI FOR TARGETING OF SOFT TISSUE TUMOUR BIOPSIES AT 3T: PRELIMINARY RESULTS. Eur Radiol 2015;25:2041-8
> Papp DF, Khanna AJ, McCarthy EF, Carrino JA, Farber AJ, Frassica FJ. Magnetic resonance imaging of soft-tissue tumors: determinate and indeterminate lesions. J Bone Joint Surg Am. 2007; 89 Suppl 3:103-15.
> Roberts CC, Liu PT, Wenger DE. Musculoskeletal tumor imaging, biopsy, and therapies: self-assessment module. AJR Am J Roentgenol. 2009; 193 Suppl 6:74-8.
> Shapeero LG, De Visschere PJ, Verstraete KL, Poffyn B, Forsyth R, Sys G, Uyttendaele D. Post-treatment complications of soft tissue tumours. Eur J Radiol. 2009; 69:209-21.
> Singh J, James SL, Kroon HM, Woertler K, Anderson SE, Davies AM. Tumour and tumour-like lesions of the patella–a multicentre experience. EurRadiol. 2009; 19:701-12.
> Vanel D, Ruggieri P, Ferrari S, Picci P, Gambarotti M, Staals E, Alberghini M. The incidental skeletal lesion: ignore or explore? Cancer Imaging. 2009, 2; 9 Spec No A:38-43.
> Vanel D. Musculoskeletal primary tumours: treatment evaluation and detection of recurrences. Cancer Imaging. 2007, 1; 7 Spec No A: 150-1.
> van der Heijden L, Gibbons CL, Dijkstra PD, Kroep JR, van Rijswijk CS, Nout RA, Bradley KM, Athanasou NA, Hogendoorn PC, van de Sande MA. The managementof diffuse-type giant cell tumour (pigmented villonodularsynovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis).J Bone Joint Surg Br. 2012; 94:882-8.
> Vanderschueren GM, Taminiau AH, Obermann WR, van den Berg-Huysmans AA, Bloem JL, van Erkel AR.The healing pattern of osteoid osteomas on computed tomography and magnetic resonance imaging after thermocoagulation. Skeletal Radiol. 2007; 36:813-21.
> van Persijn van Meerten EL, Gelderblom H, Bloem JL. RECIST revised: implications for the radiologist. A review article on the modified RECIST guideline.EurRadiol. 2010; 20:1456-67. Epub 2009 Dec 22. PubMed.
> Vermaat M, Vanel D, Kroon HM, Verbeke SL, Alberghini M, Bovee JV, Bloem JL.Vasculartumorsofbone: imaging findings. Eur J Radiol. 2011; 77:13-18.
> Vilanova JC, Woertler K, Narváez JA, Barceló J, Martínez SJ, Villalón M, Miró J. Soft-tissue tumors update: MR imaging features according to the WHO classification. EurRadiol. 2007; 17:125-38.
> Vilanova JC, Barceló J. Diffusion-weighted whole-body MR screening. Eur J Radiol. 2008; 67:440-7
Manaster BJ. Soft-Tissue Masses: Optimal Imaging Protocol and Reporting. American Journal of Roentgenology. 2013; 201:505-14.
> Weber MA, Sprengel SD, Omlor GW, Lehner B, Wiedenhöfer B, Kauczor HU, Rehnitz C. Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection. Skeletal Radiol 2015; 44:981-993.
> Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology. 2009; 253:297-316.
> Wohlgemuth WA, Wölfle K, Schuster T, Schlimok G, Bohndorf K. Hereditary vascular malformations: classification, symptoms, diagnostics and prognosis.ZentralblChir. 2012; 137:440-5.
REPORTS
COURSE REPORT – Amman Jordan ESSR-KHCC 22-23 Sept.2022 – download
PROJECTS
- A consensus paper on guidelines for imaging of soft tissue tumours, representing the viewpoint of the ESSR: in progress (correspondence to Iris-M. Noebauer-Huhmann)
- Initiative to participate in ESSR “polycenter-studies” on rare MSK tumour entities:
- Data bases on synovial sarcoma, on subcutaneous tumours, and on skeletal tumours (the latter by the Spanish skeletal radiological society [SERME], which might be extended to ESSR): in progress
- Project on Imaging presentation of extraskeletal Ewing’s sarcoma (correspondence to Violeta Vasilevska Nikodinovska )
- Project on Monoostotic Fibrous Dysplasia of the spine. MRI and CT appearance (correspondence to Andrea Baur-Melnyk)
- The subcommittee supports a multi centric study by the Research Committee and Ultrasound Subcommittee. The goal of the study is to compare MRI and US in follow-up of STT as described in “Follow-up of recurrences of limb soft tissue sarcomas in patients with localized disease: performance of ultrasound” Tagliafico A, Truini M, Spina B, Cambiaso P, Zaottini F, Bignotti B, Calabrese M, Derchi LE, Martinoli C.
Eur Radiol. 2015 Mar 21
LINKS
National Comprehensive Cancer Network (NCCN)
European Society for Medical Oncology (ESMO) Clinical Practice Guidelines
American College of Radiology (ACR) Appropriateness Criteria® – American College of Radiology
PROCEDURE TO JOIN THE SUBCOMMITTEE
Colleagues interested are very welcome to join the Subcommittee directly emailing the chairperson and attaching a short curriculum vitae.